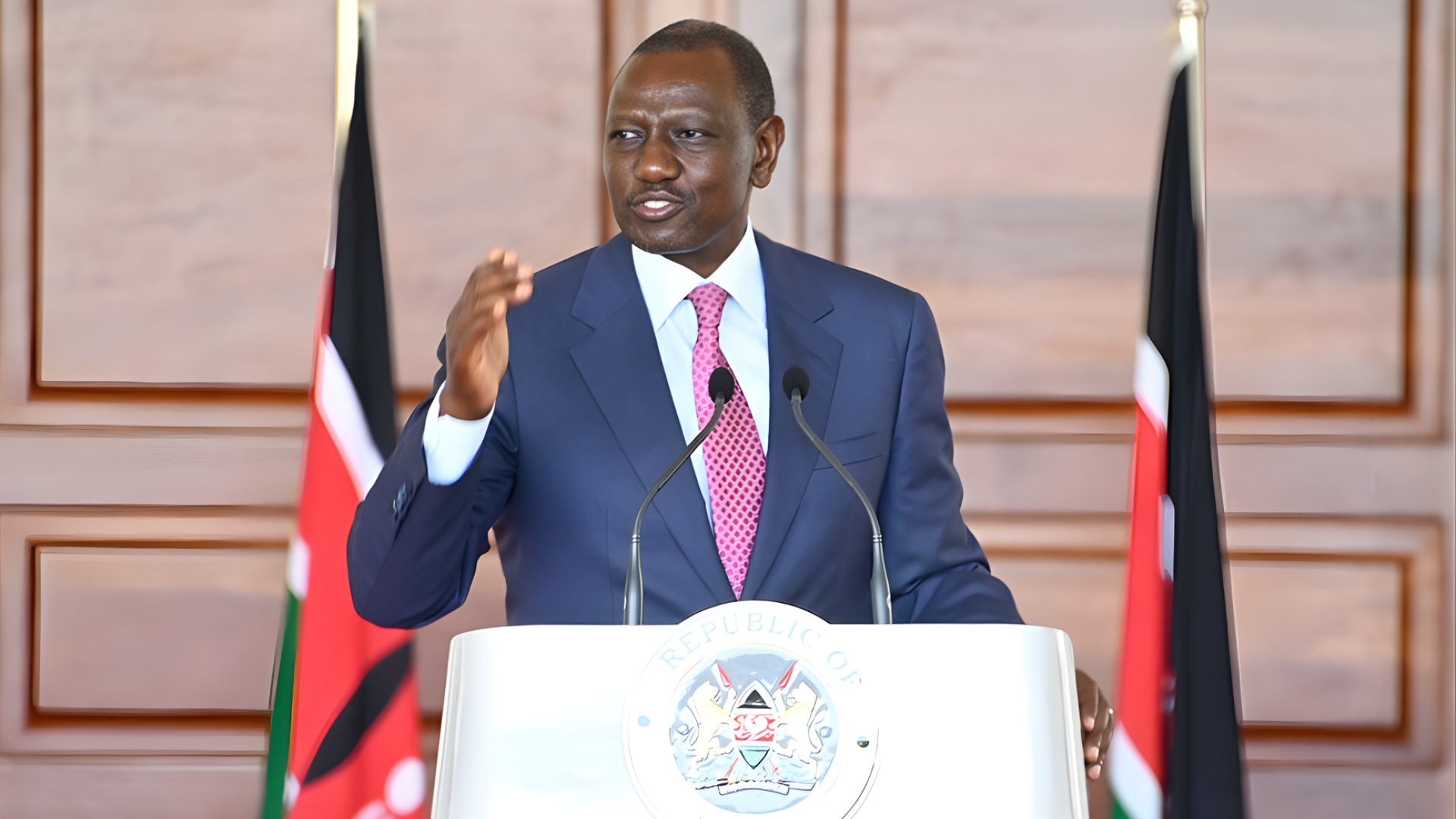
The gleaming halls of the Social Health Authority's headquarters in Nairobi's Upper Hill, where the air hums with the quiet efficiency of case managers processing enrollment forms and the faint scent of fresh printer ink from policy manuals, are about to become a beacon of relief for thousands of Kenyans who have watched their M-Pesa balances dwindle due to mistaken health premium deductions. On the morning of November 21, 2025, SHA Director General Dr. Daniel Yumbya unveiled a streamlined refund system designed to reclaim overpaid or wrongly sent premiums, a mechanism that promises to resolve the backlog of 15,000 claims accumulated since the authority's October 2024 launch. Standing before a backdrop of flowcharts illustrating the simple three-step process, Yumbya addressed a room filled with representatives from consumer protection groups, financial literacy advocates, and M-Pesa agents who had traveled from as far as Kisumu and Mombasa. "No Kenyan should lose sleep over a misplaced tap or an erroneous auto-deduction—this new system puts refunds within reach, ensuring your money works for your health, not against it," Yumbya declared, his voice carrying the reassuring tone of a physician prescribing a long-overdue remedy. "Submit your mobile money statement, your national ID, and a letter to the CEO for verification, and we'll process your claim within 14 days—no bureaucracy, no barriers."
The initiative, detailed in SHA's November 20 gazette notice and a user guide distributed to 5,000 Huduma Centres nationwide, addresses a persistent pain point in the transition from the National Health Insurance Fund to SHA, where automated deductions via M-Pesa—set at 2.75 percent of gross income for salaried workers and fixed Sh300 monthly for informal sector enrollees—have led to thousands of errors. Overpayments occur when salaries fluctuate, double deductions hit during payroll glitches, or family members accidentally send funds to the wrong till number (SHA's 222222). "I sent Sh1,500 meant for my brother's school fees to the wrong SHA code—it's been three months, and I'm chasing shadows for a refund," recounted 34-year-old single mother Fatuma Ali from Rongai, her voice laced with frustration as she held up a crumpled M-Pesa statement during the briefing. "This system gives hope—ID, statement, letter to the CEO—finally, a path without the runaround."
Yumbya's announcement, timed to coincide with SHA's first anniversary, builds on the authority's 2025 enrollment drive that has onboarded 12 million citizens, surpassing NHIF's 8 million peak. The refund process, accessible via the SHA app or Huduma portals, requires claimants to email or deliver scanned documents to ceo@sha.go.ke: a 30-day M-Pesa statement highlighting the erroneous transaction, a copy of the national ID or passport, and a self-penned letter to the CEO explaining the error and requesting reversal. "Verification takes seven days—our team cross-checks with M-Pesa till logs and SHA records," explained SHA Claims Manager Rose Wanjiku, demonstrating the portal on a large screen where a mock claim resolved in 12 clicks. "Once approved, funds reverse to the original sender's M-Pesa in 48 hours—no fees, no fines." For overpayments, refunds are capped at Sh50,000 per claim, with appeals for larger amounts routed to the SHA board.
The system's rollout addresses a backlog of 15,000 claims totaling Sh450 million since October 2024, with 40 percent from informal sector users confused by the flat Sh300 levy. "Many sent Sh600 thinking it covered two months—now they get it back, plus clarity on the Sh300 standard," Wanjiku noted, projecting stats showing 6,000 resolved since pilot in July. Ali, from Rongai, was among the first: "My Sh1,500 reversed in ten days—enough for my son's fees and a week's groceries. SHA listened when NHIF didn't."
Challenges persist: 30 percent of claims rejected for incomplete docs, rural access limited by 2G networks. SHA's response: 500 mobile clinics by December, app offline mode for statements. Consumer Federation's Stephen Mutoro: "Refunds restore faith—NHIF's 20 percent denial rate bred distrust; SHA's 85 percent approval is progress."
The process's three steps: statement scan, ID copy, CEO letter—emailed or Huduma-delivered. Verification: 7 days. Refund: 48 hours. Cap: Sh50,000. Backlog: 15,000 claims Sh450 million. For Ali: Sh1,500 reversed. In Kenya's health horizon, the system shines—a refund revolution where errors erase, and equity endures.